All for one, not one for all: The promise and challenges of personalized medicine
Personalized medicine describes treatment designed for one or more people with life-threatening conditions, such as cancer that no longer responds to chemotherapy, or infections that are resistant to multiple antibiotics.
Although personalized medicine is promising, it is labor intensive and expensive, and the pathways to approval and reimbursement are complex, as the small number of eligible patients limits the design of clinical trials. .
Here we use the latest examples of chimeric antigen receptor (CAR) T-cell therapy for advanced cancer, and bacteriophage (phage) therapy for antibiotic-resistant bacterial infections, to show how people Canadians can benefit from these personalized solutions.
Challenges that need to be overcome include ensuring equal access, and deciding who should cover the costs of these important medical advances.
CAR T-cell therapy for cancer that relapses after chemo
CAR T-cell therapy was first approved in 2017. In CAR T-cell therapy, a patient’s white blood cells are harvested and modified in a laboratory to identify and destroy a specific tumor. The modified cells are returned to the patient, where they attack the cancer.
CAR T-cell therapy has great potential to treat certain types of advanced leukemia or lymphoma. Many patients experience remission after treatment, and some even receive long-term treatment.
For example, the first CAR T-cell therapy led to an 80 percent reduction three months after treatment and 62 percent after two years. Emily Whitehead, the first pediatric patient to receive CAR T-cells, remains cancer-free 12 years after her treatment in 2012, even though her life expectancy before treatment was only a few weeks.
Bacteriophage therapy for antibiotic-resistant superbugs
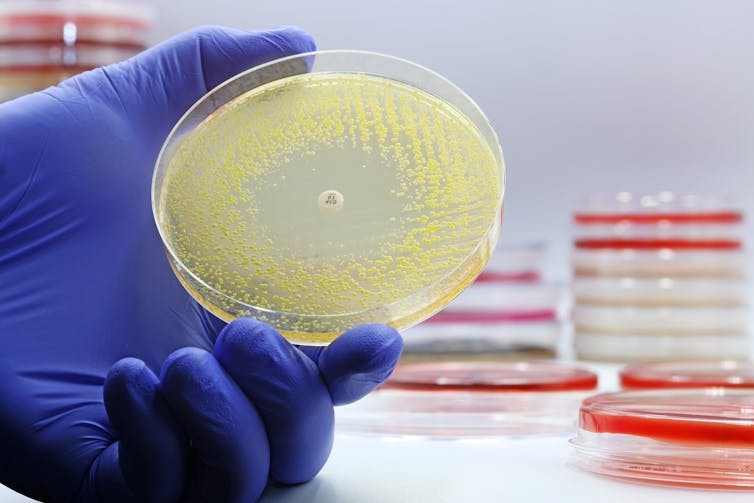
(Shutterstock)
Another patient-specific treatment uses phages: viruses that kill bacteria but are harmless to humans and animals. They were discovered a century ago by the French-Canadian microbiologist Félix d’Hérelle and were used to treat infections before the discovery of antibiotics.
As the world’s antibiotic standards continue to rise, people are turning back to treating incurable “superbug” infections.
Phages are scavengers, so it is necessary to carefully compare the bacteria that cause infection with the phages that recognize them as prey. Several types of phages are often combined in a “cocktail,” to reduce the chance that the bacteria will not be recognized by the phages.
Canada’s first modern trial of phage therapy for drug-resistant urinary tract infection (UTI) in 2023 was a success. The patient had already lost a kidney due to his infection, which could not be resolved with antibiotics alone.
In one recent example, a patient with an infection challenging his prosthetic hip was successfully treated using phage therapy.
Challenges of production, approval and reimbursement
Individual medicine is expensive. This is largely due to the fact that individualizing treatments is very complex and often limits the ability to achieve cost-effectiveness. The production methods can be standardized to some extent, but there will be features that are unique to each patient.
For example, although phages are abundant in nature and readily available, matching the correct ones to each patient’s host takes time and effort. There are few manufacturers who can prepare a phage cocktail in a short time if standard antibiotic treatment fails.
In the case of CAR T-cell therapy, the patient’s cells must be harvested and modified to target a specific tumor. The process requires strict quality control, advanced training and equipment, and a single infusion can cost more than US$350,000. Pre- and post-treatment costs can bring the actual price closer to US$1 million. This high cost places a heavy burden on the health care system and creates a significant barrier to access.

(Shutterstock)
To reduce costs associated with third-party manufacturing, Canadian researchers have begun testing new methods of developing CAR T-cell therapies directly in Canadian academic institutions.
Canada’s standard drug regulatory system was designed to approve single treatments for most patients, using evidence from large clinical trials. Personalized medicine requires a new approach that allows the approval of individual treatment for a very small group, or even a single person.
Treatments with a small number of patients can be evaluated under Health Canada’s new Notice of Compliance with Conditions (NOC/c), which allows promising treatments to reach the market with conditions. Full approval is later based on the collection of more clinical evidence.
This pathway speeds up the approval process so Canadians can get treatment for life-threatening or debilitating diseases faster. Further changes in the regulatory system may be necessary to provide an increasing number of personalized medicines.
Alternatively, Canada could follow the lead of Belgium, which took the approach of pre-adopting a large pool of individual phage, which could be combined in unique ways for each patient without and other regulatory measures. They recently published data from the first 100 cases, reporting high success rates.
Small sample sizes and a lack of individualized drug dosages can make it difficult to assess the health economic effects, which governments typically rely on for approval and reimbursement decisions. Canada has begun supplementing with real-world data/evidence from clinical centers in cases where large-scale trials are not possible. Such information includes patient or health delivery data that is already collected from a variety of sources, including electronic health records or digital health technology.
Strategies to enhance access
However, challenges remain in the way we collect and integrate information across our various provincial health care systems. The Government of Canada recently invested $20 million to improve the collection and use of real-world evidence for regulatory decision-making as part of a strategy to increase access to drugs for rare diseases , another case where the number of patients is low but the morbidity rate can be high.
New methods for evaluating the cost-effectiveness of individual medicines will also be important. Such assessments measure the prevalence of disease, the accuracy of diagnostic tests, the effectiveness of treatment, the likelihood of complications, the availability of better treatments, and the life years changed to justify the cost of treatment. Having a clearer idea of the cost-saving ratio of personalized medicine will help justify the use of scarce health care resources.
Implementing an outcomes-based reimbursement system can address cost, reimbursement, and access issues. Here, payments would only be made if the patient responded to treatment within a certain period of time. Patient assistance programs will also be important to reduce other costs. Sometimes these are offered by drug manufacturers to provide prescription drugs to eligible patients at low or no cost.
The field of personalized medicine will continue to grow, with more and more methods for more and more indications. Ensuring timely and affordable access to these treatments despite their high cost and small number of patients will be very important. Success will require collaboration between pharmaceutical companies, government agencies, insurance companies and health care facilities.
#promise #challenges #personalized #medicine
